SPRING 2019, THE EVIDENCE FORUM, WHITE PAPER
 Lindsey Murray, PhD Research Scientist Patient-Centered Research Evidera |  Elizabeth Bacci, PhD Research Scientist Patient-Centered Research Evidera |
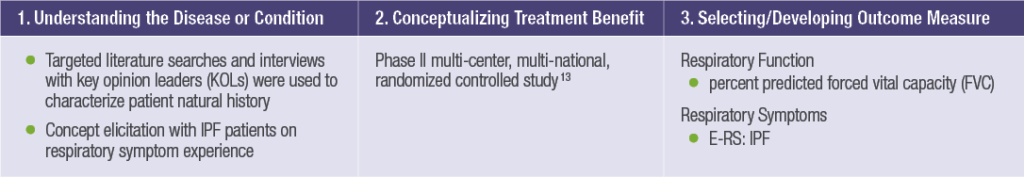
Developing clinical outcome assessment (COA) tools specific to rare diseases can be extremely challenging due to a variety of factors, including: small numbers of patients in the target indication to participate in the tool development process; heterogeneity in the disease presentation; course and response to treatment; incomplete natural history of the disease; impact on vulnerable populations; the potential association with progressive cognitive and functional impairment, and/or lack of established clinical endpoints or biomarkers.1,2 Taking these challenges into account, in the US Food and Drug Administration’s (FDA) recent draft guidance on rare diseases, Rare Diseases: Common Issues in Drug Development Guidance for Industry, the “FDA advises sponsors to consider using or modifying existing assessment measures for the disease under study because evaluating novel measures is time consuming, with potential unexpected outcomes, and evaluations initiated late in the process could delay drug development. At meetings with FDA, sponsors should discuss the availability and modification of existing clinical outcome assessments” [p. 12, lines 457-462].2 The FDA has previously published a Roadmap to Patient-Focused Outcome Measurement in Clinical Trials, which provides guidance on the steps for COA selection or development, including three key steps: 1) understanding the disease or condition; 2) conceptualizing treatment benefit; and, 3) selecting/developing the outcome measure.3 However, it can be challenging to follow this framework within a rare disease indication.
Thus, the ISPOR Rare Disease Clinical Outcomes Assessment Task Force has provided guidance on addressing the challenges to COA development within the FDA Roadmap framework, including these recommendations:
- Use multiple sources of information including clinical experts, patients, and/or caregivers to inform the natural history of the disease
- Focus on measuring common symptoms across patient subgroups, identifying short-term outcomes, and using multiple types of COAs to measure similar constructs
- Adapt existing COA measures that include symptoms of importance to the rare disease under study1
To illustrate how an existing tool can be modified and adapted for use in a rare disease population, in line with FDA expectations of COA development, the focus of this article will summarize the adaption of the Evaluating Respiratory Symptoms (E-RS®) for COPD (E-RS: COPD) for use with patients with idiopathic pulmonary fibrosis (IPF). The E-RS: COPD scale is a derivative instrument of the EXAcerbations of Chronic obstructive pulmonary disease Tool (EXACT®) used to measure the effect of treatment on the severity of respiratory symptoms in stable COPD.4,5 The instrument uses the 11 respiratory symptoms from the EXACT, including breathlessness, cough, sputum, chest congestion, chest discomfort, and chest tightness. In line with guidelines for PRO instrument development and regulatory expectations, development of the E-RS: COPD included concept elicitation interviews with COPD patients with and without a history of exacerbation, as well as extensive psychometric testing in both a natural history study and clinical trial programs.4,6 In addition, experts in pulmonary medicine, clinical research, instrument development, and drug development regulators reviewed and evaluated results throughout the development process. Confirmatory factor analysis conducted during psychometric evaluations of the instrument supported a second-order model with a general factor, representing respiratory symptom severity overall (RS-Total), and three subscales representing the three key respiratory symptoms of COPD: RS-Breathlessness, RS-Cough and Sputum, and RS-Chest Symptoms. E-RS: COPD scores were designed to serve as primary, secondary, or exploratory efficacy endpoints in clinical trials evaluating interventions to reduce the severity of respiratory symptoms of stable COPD. Both the FDA and European Medicines Agency (EMA) have published qualification statements on the E-RS: COPD.7,8 In addition, the E-RS: COPD has been incorporated into three labeling claims in Europe, supporting the qualitative and quantitative rigor of its development in line with regulatory expectations for use in COPD.
Combined with the developmental robustness of the tool, the symptoms included in the E-RS: COPD (breathlessness, cough, sputum, and chest congestion) are not unique to COPD. This makes the E-RS a good candidate for potential adaptation to other respiratory disease areas, including rare diseases. One such rare disease with a similar impact on respiratory functioning is idiopathic pulmonary fibrosis. IPF is a rare, progressive, and ultimately fatal pulmonary disease of unknown etiology with symptoms that can have a profound impact on patients’ health-related quality of life (HRQoL). The natural disease course varies; some patients experience a rapid decline in pulmonary function, others report a steady decline over a few years, and some experience stable disease interspersed with acute exacerbations.9 Increased breathlessness and cough are associated with disease progression, contributing to declines in physical functioning and HRQoL.10,11 No disease-specific patient diaries for evaluating respiratory symptoms in IPF had been developed, therefore, the E-RS: COPD tool was selected for potential adaptation.
To adapt the E-RS: COPD for use in the IPF patient population, a 2-phase qualitative and quantitative study was conducted. In Phase 1, a cross-sectional qualitative study was performed to assess and document the content validity of the E-RS: IPF; i.e., the extent to which the E-RS: COPD items adequately and accurately reflect the respiratory symptoms of IPF patients.12 Semi-structured telephone interviews were conducted with 30 adults with IPF using a combination of elicitation and cognitive interviewing techniques. The study assessed the extent to which IPF subjects would describe their respiratory symptoms differently or discuss any new respiratory symptoms not previously identified by COPD patients, as well as patient understanding of the items comprising the E-RS: COPD.12
With so many instruments already developed and validated in more common diseases ... there is a rich source of data just waiting to be tapped.
Results of this qualitative research showed four categories of respiratory symptoms that IPF patients experience: breathlessness, cough, sputum, and chest symptoms. Breathlessness and cough were the most frequently reported symptoms. Respiratory symptoms experienced by participants in this sample were mapped to the items in the E-RS: COPD. All respiratory symptoms covered by the E-RS: COPD were endorsed by ≥30% of the IPF patients. Patients’ descriptions of their respiratory symptoms were compared with the phrasing of E-RS: COPD questions and response options to determine if the wording of the items was appropriate for IPF patents. Overall, this study indicated the item content of the E-RS: COPD was appropriate for evaluating respiratory symptoms in IPF patients, and that these patients understood the content and structure of the items, thus supporting their content validity in IPF patients. No modifications to the instrument were made following these interviews.
In Phase 2, data from a Phase IIb clinical study in mild to moderate IPF patients (Parker et al. 201813) was used to evaluate the performance characteristics of the instrument, including the factor structure. Exploratory factor analysis demonstrated that a four-factor solution, indicating four respiratory symptom subscales (IPF-Breathlessness, IPF-Cough, IPF-Sputum, and IPF-Chest Symptoms), best represented the data and no overall total score was appropriate. This finding indicates the only modification of the E-RS: COPD for use in IPF patients, as the E-RS: COPD is comprised of three factors and an overarching total score. Using this scaling structure, instrument reliability, validity, and responsiveness to change over time were assessed. These analyses indicated that the E-RS: IPF is a valid, reliable, and sensitive measure, although additional research is needed to confirm these findings in a separate patient population. Based on the results of this study, the E-RS: IPF may be a useful instrument for evaluating respiratory symptoms of IPF. This instrument was successfully adapted for use in a rare disease population, avoiding potentially significant challenges if an entirely new instrument was developed.
Rare diseases present unique challenges in clinical trial design and in selection of COAs that can support claims in medical product labeling. Although guidance exists on suggestions for addressing these challenges, there is no “one-fit” solution to COA selection in a rare disease. Adapting existing instruments for use in rare diseases is one possible solution to the many challenges encountered in the development of rare disease treatments. Any advantage that can help simplify the process, efficiently utilize sparse and valuable resources, and potentially provide faster access to these specialized treatments that can help increase quality and length of life is worth investigating. With so many instruments already developed and validated in more common diseases that may include items relevant to other disease areas or populations, there is a rich source of data just waiting to be tapped. This article illustrates how an existing measure was modified for use in a rare disease population. More information on the EXACT, E-RS: COPD, and E-RS: IPF can be found here.
References
- Benjamin K, Vernon MK, Patrick DL, et al. Patient-Reported Outcome and Observer-Reported Outcome Assessment in Rare Disease Clinical Trials: An ISPOR COA Emerging Good Practices Task Force Report. Value Health. 2017 Jul – Aug;20(7):838-855. doi: 10.1016/j.jval.2017.05.015.
- US Food and Drug Administration. Rare Diseases: Early Drug Development and the Role of Pre-IND Meetings Guidance for Industry. October 2018. Available at: https://www.fda.gov/downloads/Drugs/GuidanceComplianceRegulatoryInformation/Guidances/UCM623293.pdf. Accessed February 15, 2019.
- US Food and Drug Administration. Roadmap to Patient-Focused Outcome Measurement in Clinical Trials. 2015. Available at: https://www.fda.gov/downloads/drugs/developmentapprovalprocess/drugdevelopmenttoolsqualificationprogram/ucm370174.pdf. Accessed February 15, 2019.
- Leidy NK, Sexton CC, Jones PW, Notte SM, Monz BU, Nelsen L, Goldman M, Murray LT, Sethi S. Measuring Respiratory Symptoms in Clinical Trials of COPD: Reliability and Validity of a Daily Diary. Thorax. 2014 May;69(5):443-449. doi: 10.1136/thoraxjnl-2013-204428.
- Leidy NK, Murray LT. Patient-Reported Outcome (PRO) Measures for Clinical Trials of COPD: the EXACT and E-RS. COPD. 2013 Jun;10(3):393-398. doi: 10.3109/15412555.2013.795423.
- Leidy NK, Murray LT, Monz BU, Nelsen L, Goldman M, Jones PW, Dansie EJ, Sethi S. Measuring Respiratory Symptoms of COPD: Performance of the EXACT-Respiratory Symptoms Tool (E-RS) in Three Clinical Trials. Respir Res. 2014 Oct 7;15(1):124. doi: 10.1186/s12931-014-0124-z.
- European Medicines Agency, Product Development Scientific Support Department. Draft Qualification Opinion of Qualification of Exacerbations of Chronic Pulmonary Disease Tool (EXACT), and EXACT-Respiratory Symptoms Measure (E-RS) for Evaluating Treatment Outcomes in Clinical Trials in COPD. 10 April 2015. Available at: http://www.ema.europa.eu/docs/en_GB/document_library/Regulatory_and_procedural_guideline/2015/04/WC500185442.pdf. Accessed February 6, 2019.
- US Food and Drug Administration. Attachment to Guidance on Qualification Process for Drug Development Tools. Draft Guidance on Evaluating Respiratory Symptoms in Chronic Obstructive Pulmonary Disease, a Patient-Reported Outcome Instrument for the Measurement of Severity of Respiratory Symptoms in Stable Chronic Obstructive Pulmonary Disease: Qualification for Exploratory Use. March 2016. Available at: https://www.fda.gov/downloads/Drugs/GuidanceComplianceRegulatoryInformation/Guidances/UCM489526.pdf. Accessed February 6, 2019.
- Raghu G, Collard HR, Egan JJ, et al.; ATS/ERS/JRS/ALAT Committee on Idiopathic Pulmonary Fibrosis. An Official ATS/ERS/JRS/ALAT Statement: Idiopathic Pulmonary Fibrosis: Evidence-Based Guidelines for Diagnosis and Management. Am J Respir Crit Care Med. 2011 Mar 15;183(6):788-824. doi: 10.1164/rccm.2009-040GL.
- Olson AL, Brown KK, Swigris JJ. Understanding and Optimizing Health-Related Quality of Life and Physical Functional Capacity in Idiopathic Pulmonary Fibrosis. Patient Relat Outcome Meas. 2016 May 17;7:29-35. doi: 10.2147/PROM.S74857. eCollection 2016.
- Swigris JJ, Kuschner WG, Jacobs SS, Wilson SR, Gould MK. Health-Related Quality of Life in Patients with Idiopathic Pulmonary Fibrosis: A Systematic Review. Thorax. 2005 Jul;60(7):588-594.
- Bacci ED, O’Quinn S, Leidy NK, Murray L, Vernon M. Evaluation of a Respiratory Symptom Diary for Clinical Studies of Idiopathic Pulmonary Fibrosis. Respir Med. 2018 Jan;134:130-138. doi: 10.1016/j.rmed.2017.11.011. Epub 2017 Nov 26.
- Parker JM, Glaspole IN, Lancaster LH, et al. A Phase 2 Randomized Controlled Study of Tralokinumab in Subjects with Idiopathic Pulmonary Fibrosis. Am J Respir Crit Care Med. 2018 Jan 1;197(1):94-103. doi: 10.1164/rccm.201704-0784OC.
For more information, please contact
[email protected] or [email protected]