FALL 2020, THE EVIDENCE FORUM, WHITE PAPER
 Andreas Freitag, MD, MSC Research Scientist Evidence Synthesis, Modeling & Communication Evidera, a PPD business |  Ike Iheanacho, MBBS Senior Director and Senior Research Scientist Evidence Synthesis, Modeling & Communication Evidera, a PPD business |
While rare diseases are individually uncommon, they collectively represent a major burden to society as well as to the patients concerned. Overall, more than 7,000 such diseases are known, affecting an estimated total of 30 million to 40 million people in the European Union (EU) and 400 million worldwide.1,2 The definition of rare diseases differs across jurisdictions, although it is typically based on prevalence estimates. For example, rare diseases are defined as those affecting <200,000 people in the United States (US),3 and <1 in 2,000 people in the EU,4 with conditions affecting <1 in 50,000 in the EU being additionally classified as “ultra-rare.”5 Patients with rare diseases face immense difficulties in accessing treatment,6 particularly due to the lack of effective options for many conditions. Where therapies do exist, challenges associated with current regulatory and reimbursement frameworks contribute to the limited access to care. Here we discuss the current state of moves to address this situation.
What's the Problem?
Traditionally, the very small patient populations with each rare condition have made rigorous clinical trials of new therapies unfeasible or financially unviable.7 The conduct of clinical trial programs is further hampered by a lack of fundamental knowledge about key aspects of many rare diseases, including their epidemiology and natural history. Also, the heterogenous disease landscape with regard to their pathophysiology, symptom presentation, and disease characteristics can make it particularly difficult to recruit enough patients to sufficiently power a clinical trial.8
The resulting low level research activity and associated lack of specific licensed and reimbursed treatments for many rare diseases has promoted the use of the term “orphan disease” when referring to such conditions.6 To address these evidence and therapeutic gaps in rare diseases, legal frameworks have been established in many countries to promote the development and commercialization of treatments (often called “orphan drugs”).
Incentives for Orphan Drug Development
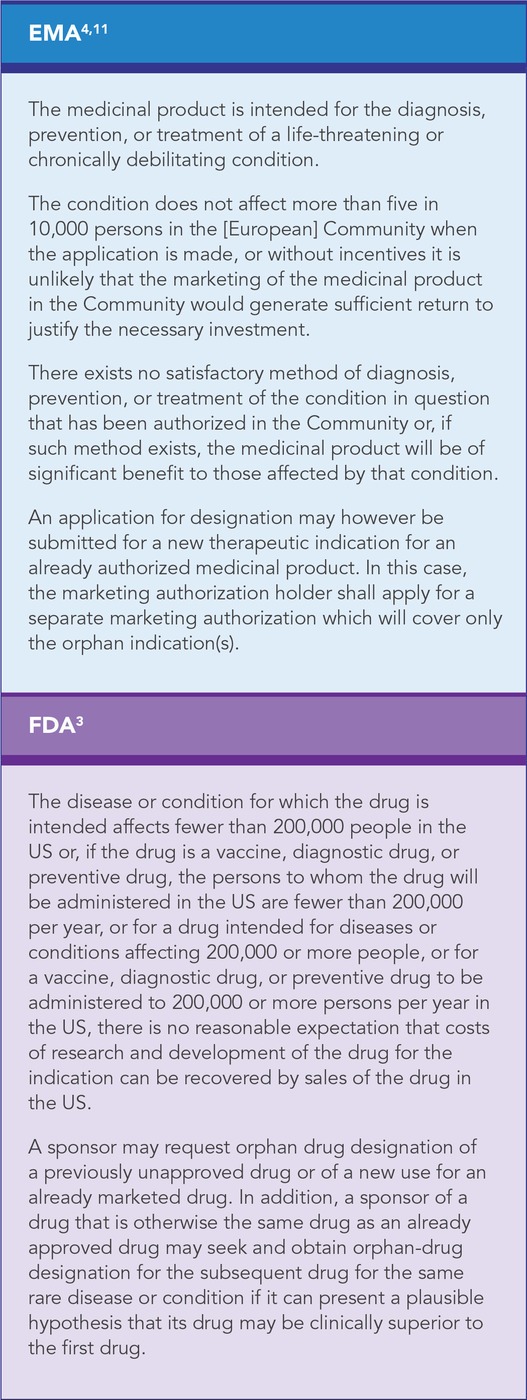
Understanding, awareness, and interest concerning rare diseases have grown in recent decades, resulting in various policies and incentives to encourage manufacturers to develop treatments for these conditions.1,6 Orphan designation (or status) was formally defined in the US through the Orphan Drug Act 1983, and in the EU as part of the specialized pathway for application of orphan medicinal product (OMP) designation (based on Regulation (EC) No. 141/2000).4,9 This legislation dictates that for a drug to be awarded orphan designation, it must meet specific criteria focusing on a condition’s prevalence, the absence of existing treatment options, and the high costs of drug development (which the manufacturer may not be able to recoup through sales) (See Table 1). However, orphan designation does not confer marketing authorization. Instead, such designation represents part of the research and development stage of drug development by providing a framework for evaluating a drug’s efficacy and safety profile.
Once orphan drug status has been awarded, both the European Medicines Agency (EMA) and the United States Food and Drug Administration (FDA) support drug development for rare diseases through financial incentives such as tax credits, the waiver of future fees, or market exclusivity (for 7 years in the US and 10 years in the EU). Regulatory agencies also provide support through scientific advice, particularly on the conduct of tests and trials to demonstrate the efficacy, safety, and quality of the drug being considered for marketing authorization.10 Designated drugs may be considered for specific approval pathways that are not limited to orphan treatments (e.g., the FDA’s accelerated approval pathway or EMA’s conditional approval).
Requirements for Regulatory and Reimbursement Assessment
Regulatory and reimbursements pathways follow standardized processes to assess candidate new medicines and depend heavily on evaluation of clinical trial data. However, these two types of pathways differ from each other and across territories with regards to their evidence requirements for these products. This can pose major challenges for both manufacturers and authorities, especially in the context of rare diseases, where the value of a drug may not be easy to demonstrate through traditional clinical and cost-effectiveness measures.
Regulatory bodies, such as the EMA and FDA, mainly consider evidence on the therapeutic effects and safety of a drug. The need for such data may help explain why, despite the significant increase in the number of granted orphan designations in recent years, only a few of these have ultimately resulted in licensed products.
An even broader range of evidence is generally needed to support reimbursement submissions, including comparative efficacy and safety and, often, the cost effectiveness of a drug in a local healthcare setting. Some health technology assessment (HTA) bodies also require good quality-of-life data to demonstrate the burden of a disease and the impact of its treatment on patient-reported outcomes.12 In many instances, orphan drugs go through the same assessment processes as those without this status. The extensive requirements for these evaluations can pose problems for manufacturers’ evidence-generation strategies for orphan drugs, and this may contribute to the lack of HTA submissions for such treatments.13,14 Specific frameworks have emerged in recent years to specifically address such challenges.
Demonstrating Clinical Benefit
Consideration of clinical trial evidence remains the cornerstone of technology assessments both for orphan and non-orphan drugs. However, demonstrating the effectiveness of an orphan drug can be difficult given the lack of knowledge of the pathophysiology of many diseases, difficulties in recruiting enough patients for clinical trials, and a general lack of established active comparators. Many trials often also lack well-defined clinical endpoints, which is compounded by the often short follow-up duration in such studies. Surrogate endpoints are frequently used in clinical studies in support of applications for marketing
authorization and can be helpful in identifying clinical benefits in circumstances where small sample sizes preclude demonstrating definitive effects on longer-term or hard clinical endpoints, such as disease progression or survival.15 However, the correlation between surrogate endpoints and hard clinical endpoints is often unclear and there may be insufficient data for endpoint validation.16-18
In light of these limitations, real-world evidence is increasingly used as a source of long-term clinical data or to facilitate researching treatments for rare diseases for which clinical trial data are often sparse.19
Demonstrating Cost Effectiveness
Conducting health economic evaluations of potential treatments for rare diseases may be hard due to challenges similar to those encountered when aiming to establish a clinical benefit.14,20 Also, companies conducting such evaluations to seek reimbursement for their orphan drugs are often confronted with an unfavourable incremental cost-effectiveness ratio (ICER) that reflects high treatment costs and uncertainties around the clinical benefit. In addition, there is general acknowledgement by HTA bodies, such as the National Institute for Health and Care Excellence (NICE) and the Scottish Medicines Consortium (SMC), that quality-adjusted life years (QALYs) – a standard measure of treatment effect – do not necessarily capture all elements needed to adequately and comprehensively demonstrate the added value of orphan drugs. Accordingly, in addition to accepting higher ICERs, NICE and the SMC commonly consider other evidence sources, such as patient experience, during the evaluation process.21
Differences in HTA Requirements
Difficulties in preparing reimbursement submissions due to differences between HTA bodies in their evidence requirements (e.g., regarding the acceptability of surrogate endpoints or the need for patient-reported, as well as clinical, outcomes) may be compounded by differences in decision-making criteria across these bodies. Research suggests that these variations in assessing “value” have led to discrepancies in access to care across jurisdictions.14 For example, a survey conducted in 2010 across EU member states found, among a sample of 60 orphan drugs assessed for reimbursement, the approval rate ranged from 25% in Greece and 33% in Spain to over 90% in France.22 Consequently, manufacturers seeking reimbursement for a treatment for a rare disease may have to demonstrate multiple disparate aspects of its value in different territories while simultaneously managing the implications of its high price.
Ethics and Equity of Access
The challenges in the assessment, and therefore the limited availability, of treatments for rare diseases raises ethical questions about how much a society or healthcare system is prepared to pay for the treatment of people with these conditions. With ICERs for orphan drugs often being above typical willingness-to-pay thresholds, some commentators have expressed concerns that increasing the allocation from a finite healthcare budget to orphan drugs may reduce overall population health.23 Of note, however, some countries, such as France and Italy, tend to reimburse even highly priced orphan drugs, due to the relatively small patient population involved.20,24
To address uncertainties around the cost effectiveness of treatments and give patients access to treatment as early as possible, jurisdictions could grant conditional reimbursement. Under such arrangements, a drug is reimbursed initially for a pre-specified period during which manufacturers can collect and present additional data to inform a final decision on reimbursement. However, critics of such provisions argue that even if the ICER remains unfavourable despite new evidence, the initial positive reimbursement decisions are rarely changed, owing to political considerations.23
Frameworks to Address the Challenges
To address reimbursement challenges for orphan drugs, regulatory and HTA bodies have established assessment frameworks specific to rare diseases or those with a high unmet need. Examples include the Highly Specialised Technology (HST) framework at NICE and the ultra-orphan medicines pathway of the SMC. Furthermore, international collaborations aim to share experiences regarding clinical trial design and risk-management strategies for long-term safety issues (e.g., EMA and the FDA) or to coordinate access to orphan drugs (e.g., HTA agencies across Europe).
What’s Still Needed?
Despite the long-standing initiatives for orphan drugs, barriers to progress in the development and approval of orphan drugs still exist, and in many conditions, patients’ needs are yet to be adequately addressed. Consequently, expert opinion has highlighted various proposals to improve access to care.
First, clinical trial designs need to address the methodological limitations posed by rare, and particularly ultra-rare, diseases. Broader patient population criteria and large, international collaborations could help recruit enough patients to sufficiently power a trial. Although surrogate endpoints are increasingly accepted for regulatory and reimbursement assessments, these should be validated where possible and trial follow-up durations should be extended to also consider hard clinical endpoints or patient-relevant outcomes. This would help ensure that regulatory and reimbursement decisions are based on measures that are relevant to patients.
Second, evaluation frameworks should be further adapted to acknowledge the challenges posed in evidence generation for rare diseases. In the absence of sufficient clinical trial data, real-world evidence should be given more weight in the evaluation process. For example, the FDA launched its Real-World Evidence Program in 2018 to support evidence generation on the safety and effectiveness of medicines, as well as the use of such data in regulatory decisions.25 In the EU, there have been similar efforts, through establishing standardized patient registries to generate uniform evidence to support benefit-risk evaluations of drugs.26 There should also be more emphasis on alternative ways of assessing “value” beyond the usual evaluations of clinical effects and cost effectiveness by taking into account patient experience and complex solutions (e.g., multi-component strategies that go beyond pharmacological therapies in isolation). There is also the need to more holistically take quality of life and the impact on family members and caregivers into account given the high burden of rare diseases.21 While decision makers are increasingly recognizing the importance of incorporating such elements, particularly when robust clinical data are sparse, further changes of assessment processes are required to fully, transparently, and fairly address such “social value judgements.”27
Third, regulatory and HTA agencies need to increase their collaboration to help ensure they can evaluate and share relevant data, develop clear methodological standards, and establish transparent pathways for the approval and reimbursement of orphan drugs. In addition, changes to reimbursement and funding methods, such as conditional approval and merging healthcare and social care budgets, may be required to increase early access to care.
Conclusions
With regard to rare diseases, manufacturers and decision makers continue to face major challenges in understanding the conditions, appropriate evidence generation, and adaptation of regulatory and HTA processes to ensure timely approval and availability of treatments. In this context, the needs of patients with such conditions are often inadequately addressed. These therapeutic gaps call for improvements in the design and conduct of clinical trials, the increased use of real-world evidence to inform decision making where there is a lack of high-quality trial evidence, and further efforts to establish value frameworks that go beyond traditional HTA considerations.
References
- Harari S. Why We Should Care About Ultra-Rare Disease. Eur Respir Rev. 2016 Jun;25(140):101-3. doi: 10.1183/16000617.0017-2016.
- US Government Accountability Office. Orphan Drugs: FDA Could Improve Designation Review Consistency; Rare Disease Drug Development Challenges Continue. 2018 Nov 30. Available at: https://www.gao.gov/products/GAO-19-83. Accessed September 9, 2020.
- US Food and Drug Administration (FDA). 21 CFR § 316.20 and § 316.21. Available at: https://www.accessdata.fda.gov/scripts/cdrh/cfdocs/cfcfr/CFRSearch.cfm?CFRPart=316. Accessed: September 9, 2020.
- EUR-Lex. Regulation (EC) No 141/2000 of the European Parliament and of the Council. Available at: https://eur-lex.europa.eu/legal-content/EN/TXT/?uri=CELEX%3A32000R0141. Accessed September 10, 2020.
- EUR-Lex. Regulation (EU) No 536/2014 of the European Parliament and of the Council. Available at: https://eur-lex.europa.eu/legal-content/EN/TXT/?uri=celex%3A32014R0536. Accessed September 10, 2020.
- European Lung Foundation. Rare and Orphan Lung Disease. Available at: https://www.europeanlung.org/en/lung-disease-and-information/lung-diseases/rare-and-orphan-lung-disease. Accessed September 9, 2020.
- Richter T, Janoudi G, Amegatse W, Nester-Parr S. Characteristics of Drugs for Ultra-Rare Diseases versus Drugs for Other Rare Diseases in HTA Submissions Made to the CADTH CDR. Orphanet J Rare Dis. 2018 Feb 1;13(1):15. doi: 10.1186/s13023-018-0762-1.
- Augustine EF, Adams HR, Mink JW. Clinical Trials in Rare Disease: Challenges and Opportunities. J Child Neurol. 2013 Sep;28(9):1142-50. doi: 10.1177/0883073813495959.
- US Food and Drug Administration (FDA). Orphan Drug Act of 1983, 96 STAT. 2049. Available at: https://www.fda.gov/media/99546/download. Accessed September 9, 2020.
- European Commission. Inventory of Union and Member State Incentives to Support Research Into, and the Development and Availability of, Orphan Medicinal Products – State of Play 2015. Available at: https://ec.europa.eu/health/sites/health/files/files/orphanmp/doc/orphan_inv_report_20160126.pdf. Accessed September 9, 2020.
- Official Journal of the European Communities. Commission Regulation (EC) No 847/2000. Available at: https://eur-lex.europa.eu/LexUriServ/LexUriServ.do?uri=OJ:L:2000:103:0005:0008:en:PDF. Accessed September 9, 2020.
- Basch E, Bennett AV. Patient-Reported Outcomes in Clinical Trials of Rare Diseases. J Gen Intern Med. 2014 Aug;29 Suppl 3: S801-3. doi: 10.1007/s11606-014-2892-z.
- European Medicines Agency. EMA-HTA Workshop: Bringing Together Stakeholders for Early Dialogue in Medicines Development. 2013. Available at: https://www.ema.europa.eu/en/documents/report/report-european-medicines-agency/health-technology-assessment-body-workshop-parallel-scientific-advice-drug-development-26-november_en.pdf. Accessed September 10, 2020.
- Tordrup D, Tzouma V, Kanavos P. Orphan Drug Considerations in Health Technology Assessment in Eight European Countries. Rare Diseases and Orphan Drugs. 2014;1(3).
- Kesselheim AS, Myers JA, Avorn J. Characteristics of Clinical Trials to Support Approval of Orphan vs Nonorphan Drugs for Cancer. JAMA. 2011 Jun 8;305(22):2320-6. doi: 10.1001/jama.2011.769.
- Bolignano D, Pisano A. Good-Quality Research in Rare Diseases: Trials and Tribulations. Pediatr Nephrol. 2016 Nov;31(11):2017-23. doi: 10.1007/s00467-016-3323-7. Epub 2016 Jan 27.
- Picavet E, Cassiman D, Hollak CE et al. Clinical Evidence for Orphan Medicinal Products – A Cause for Concern? Orphanet J Rare Dis. 2013 Oct 16;8: 164. doi: 10.1186/1750-1172-8-164.
- Joppi R, Bertele V, Garattini S. Orphan Drugs, Orphan Diseases. The First Decade of Orphan Drug Legislation in the EU. Eur J Clin Pharmacol. 2013 Apr;69(4):1009-24. doi: 10.1007/s00228-012-1423-2. Epub 2012 Oct 23.
- Makady A, van Veelen A, Jonsson P, et al. Using Real-World Data in Health Technology Assessment (HTA) Practice: A Comparative Study of Five HTA Agencies. Pharmacoeconomics. 2018 Mar;36(3):359-368. doi: 10.1007/s40273-017-0596-z.
- Gammie T, Lu CY, Ud-Din Babar Z. Access to Orphan Drugs: A Comprehensive Review of Legislations, Regulations and Policies in 35 Countries. PLoS One. 2015 Oct 9;10(10): e0140002. doi: 10.1371/journal.pone.0140002. eCollection 2015.
- Nicod E, Annemans L, Bucsics A et al. HTA Programme Response to the Challenges of Dealing with Orphan Medicinal Products: Process Evaluation in Selected European Countries. Health Policy. 2019 Feb;123(2):140-151. doi: 10.1016/j.healthpol.2017.03.009. Epub 2017 Mar 28.
- EURORDIS. Survey: Patients’ Access to Orphan Drugs in Europe. Inventory of Access and Prices or Orphan Drugs Across Europe: A Collaborative Work Between National Alliances on Rare Diseases & Eurordis. Available at: https://www.eurordis.org/content/survey-patients%E2%80%99-access-orphan-drugs-europe. Accessed September 9, 2020.
- Simoens S, Picavet E, Dooms M, Cassiman D, Morel T. Cost-Effectiveness Assessment of Orphan Drugs: A Scientific and Political Conundrum. Appl Health Econ Health Policy. 2013 Feb;11(1):1-3. doi: 10.1007/s40258-012-0004-y.
- Dupont AG, Van Wilder PB. Access to Orphan Drugs Despite Poor Quality of Clinical Evidence. Br J Clin Pharmacol. 2011 Apr;71(4):488-96. doi: 10.1111/j.1365-2125.2010.03877.x.
- US FDA. Framework for FDA’s Real-World Evidence Program. 2018 Dec. Available at: https://www.fda.gov/media/120060/download. Accessed September 9, 2020.
- European Medicines Agency. Patient Registries. Available at: https://www.ema.europa.eu/en/human-regulatory/post-authorisation/patient-registries. Accessed September 9, 2020.
- Angelis A, Lange A, Kanavos P. Using Health Technology Assessment to Assess the Value of New Medicines: Results of a Systematic Review and Expert Consultation Across Eight European Countries. Eur J Health Econ. 2018 Jan;19(1):123-152. doi: 10.1007/s10198-017-0871-0. Epub 2017 Mar 16.
For more information, please contact
[email protected] or [email protected].